Proper labeling is paramount in the medical field, as it safeguards patient safety and prevents blood testing and transfusion errors. By following the best practices outlined here, healthcare professionals can streamline their workflow, minimize the risk of misidentification, and enhance patient care.
Table of Contents
- 1 Understanding Blood Collection Tubes
- 2 Types of Blood Collection Tubes
- 3 Importance of Labeling Blood Collection Tubes
- 4 When to Label Blood Collection Tubes
- 5 Guidelines for Labeling Blood Collection Tubes
- 6 Final Thoughts
- 7 FAQs
- 7.1 What are blood collection tubes used for?
- 7.2 When Should Blood Specimens Be Labeled?
- 7.3 When and Where Should Blood Bottles Be Labeled?
- 7.4 When Should You Label the Blood Specimens You Obtain?
- 7.5 When Should Collection Tubes Be Labeled?
- 7.6 What Are the Requirements for Labeling Blood Collection Tubes?
- 8 You May Also Read
Understanding Blood Collection Tubes
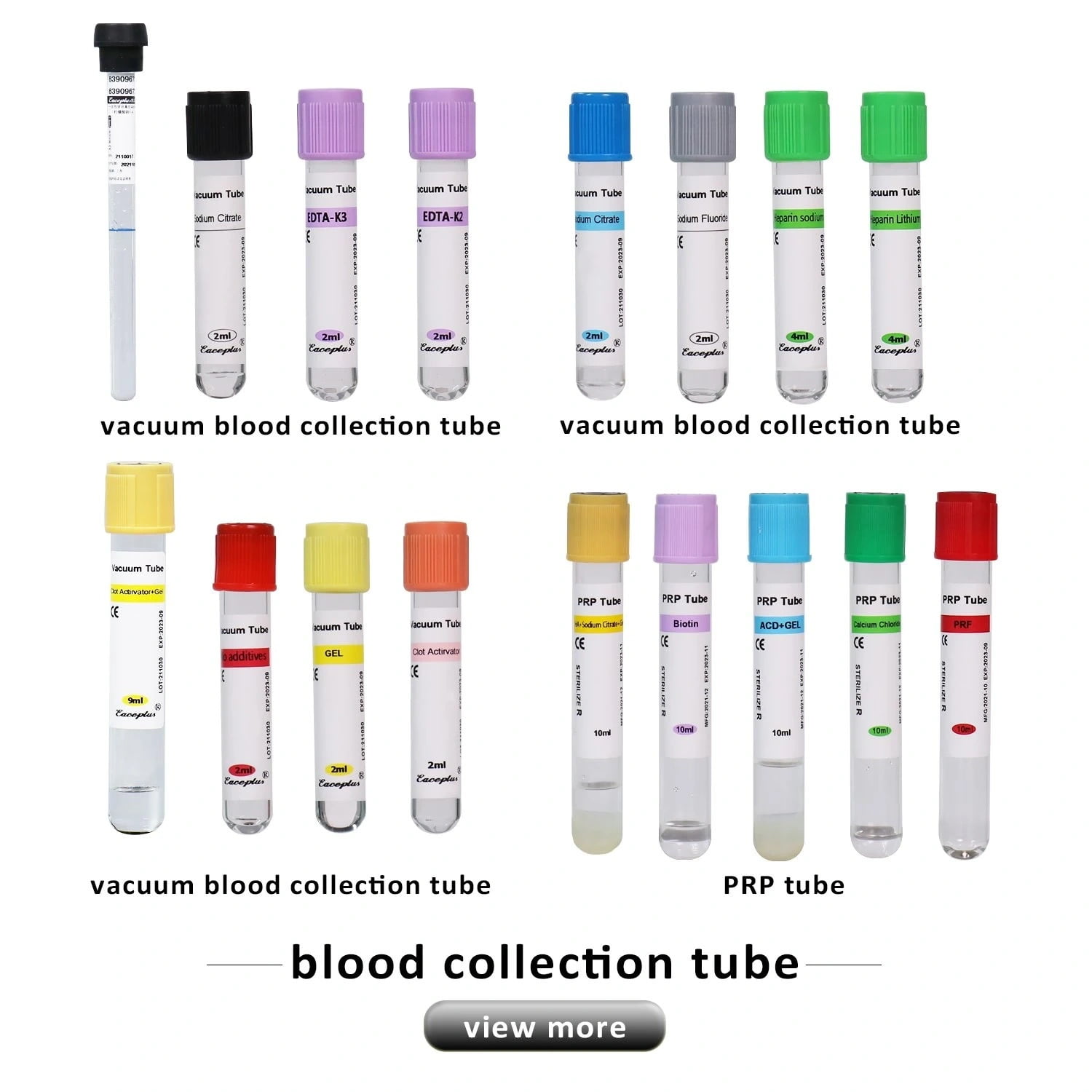
Blood collection tubes are essential tools in clinical laboratories for collecting and transporting blood samples for various tests. These tubes come in different colors, each indicating specific additives that affect how the blood sample is processed. Labeling these tubes is crucial to avoid misidentification, which can lead to incorrect diagnoses and treatment plans.

Types of Blood Collection Tubes
- Red-Top Tubes: No additives; used for serum tube.
- Lavender-Top Tubes: Contain EDTA; used for hematology tests.
- Blue-Top Tubes: Contain sodium citrate, used for coagulation studies.
- Green-Top Tubes: Contain heparin tube, used for plasma tests.
- Gray-Top Tubes: Contain sodium fluorid, used for glucose testing.
- Purple-Top Tube: EDTA (ethylenediaminetetraacetic acid)
- Yellow-Top Tube: ACD (acid-citrate-dextrose) solution
Each tube type serves a specific purpose, and understanding these differences is vital for proper labeling and handling.
Importance of Labeling Blood Collection Tubes
Labeling blood collection tubes accurately is crucial for ensuring patient safety and the integrity of diagnostic results. Mislabeling can lead to catastrophic consequences, such as incorrect diagnoses, inappropriate treatments, and even life-threatening situations for patients. Blood collection is fraught with potential errors, and proper labeling is the first defense in mitigating these risks. Labeling blood collection tubes accurately is crucial for several reasons:
- Patient Safety: Mislabeling can lead to incorrect test results, risking patient safety.
- Traceability: Proper labels allow for easy tracking of samples throughout the laboratory process.
- Regulatory Compliance: Many healthcare regulations require strict adherence to labeling protocols to maintain accreditation.
This efficiency ultimately results in improved patient care, as timely diagnosis and treatment are critical in many medical situations. Thus, proper labeling in blood collection cannot be overstated. It is a fundamental aspect of quality patient care.
When to Label Blood Collection Tubes
The timing of when blood collection tubes should be labeled is debated among healthcare professionals. However, guidelines and best practices have emerged based on clinical studies and expert opinions.

Current Best Practices
- In the Presence of the Patient: Most regulatory bodies recommend labeling blood collection tubes in the patient’s presence. This practice ensures the healthcare provider can confirm the patient’s identity before collecting the sample.
- After Collection: The majority consensus among North American regulators is that tubes should be labeled immediately after blood collection while still in front of the patient. This practice minimizes errors associated with mislabeled or unlabeled specimens.
- Pre-labeling Considerations: Some experts argue that labeling tubes before drawing blood can be beneficial if automated labeling systems are in place. This method can reduce human error and streamline the process by ensuring each tube is specifically designated for a patient.
Survey Insights
A survey conducted among healthcare professionals revealed that :
- 66% believe tubes should be labeled after collecting blood while in the presence of the patient.
- 29% support labeling before drawing blood.
- Only 5% advocate for labeling before meeting the patient
These results highlight a strong preference for post-collection labeling to enhance accuracy and safety.
Guidelines for Labeling Blood Collection Tubes
Information to Include
When labeling blood collection tubes, it is crucial to include specific information to ensure proper identification:
- Patient’s Full Name: Ensure it matches the identification documents.
- Unique Identifier: This could be a medical record number or date of birth.
- Date and Time of Collection: Essential for time-sensitive tests.
- Type of Sample Collected: Indicate if it’s serum, plasma, etc.
- Test Requested: If applicable, specify which tests are being performed.
Labeling Techniques
- Handwritten Labels: Ensure legibility and accuracy when writing directly on the tube.
- Automated Labeling Systems: Utilize technology where available to minimize human error.
Final Thoughts
In summary, properly labeling blood collection tubes is a critical component of phlebotomy practices that directly impacts patient safety and laboratory efficiency. The consensus among healthcare professionals supports labeling tubes immediately after collection while ensuring this process occurs before the patient. By adhering to established guidelines and incorporating best practices into daily routines, healthcare providers can significantly reduce the risk of errors associated with mislabeled specimens.
FAQs
What are blood collection tubes used for?
Blood collection tubes are used to collect, transport, and store blood samples for laboratory testing. Different tubes contain various additives that help preserve the sample or facilitate specific types of tests.
When Should Blood Specimens Be Labeled?
Blood specimens should be labeled immediately after collection while still in the patient’s presence. This practice minimizes the risk of mislabeling and ensures accurate identification before the patient departs, aligning with regulatory guidelines prioritizing patient safety.
When and Where Should Blood Bottles Be Labeled?
Blood bottles must be labeled at the point of care, specifically in front of the patient. This ensures that the healthcare provider can confirm the patient’s identity and that all relevant information is accurately recorded before leaving the collection site.
When Should You Label the Blood Specimens You Obtain?
Labeling blood specimens immediately after obtaining them while still in the patient’s presence would be best. This prevents errors associated with labeling after leaving the patient, which can lead to confusion and misidentification of samples.
When Should Collection Tubes Be Labeled?
Collection tubes should be labeled right after blood collection tube and before dismissing the patient. This ensures that each tube is correctly matched to its corresponding patient, reducing the risk of mislabeling and ensuring accurate test results.
What Are the Requirements for Labeling Blood Collection Tubes?
Labeling requirements for blood collection tubes include providing the patient’s full name, a unique identifier (like date of birth), date and time of collection, and initials of the person collecting the sample. Labels must be clear and securely affixed to prevent loss or confusion.
You May Also Read
- Best Blood Collection Tubes for PRP
- Types of Blood Collection Tubes and Their Uses
- What is a Serum Blood Collection Tube?
- How to use a Micro Blood Collection Tube to Collect Blood?
- The Power of Sodium Citrate Blood Collection Tubes
- The Materials and Additives used in Vacuum Blood Collection Tubes
- A Guide to Choosing Quality Blood Collection Tubes
If you enjoyed this article, please subscribe to our YouTube channel. We provide product video tutorials. You can also follow us on Instagram and Facebook to stay up to date with new updates, news and special deals.