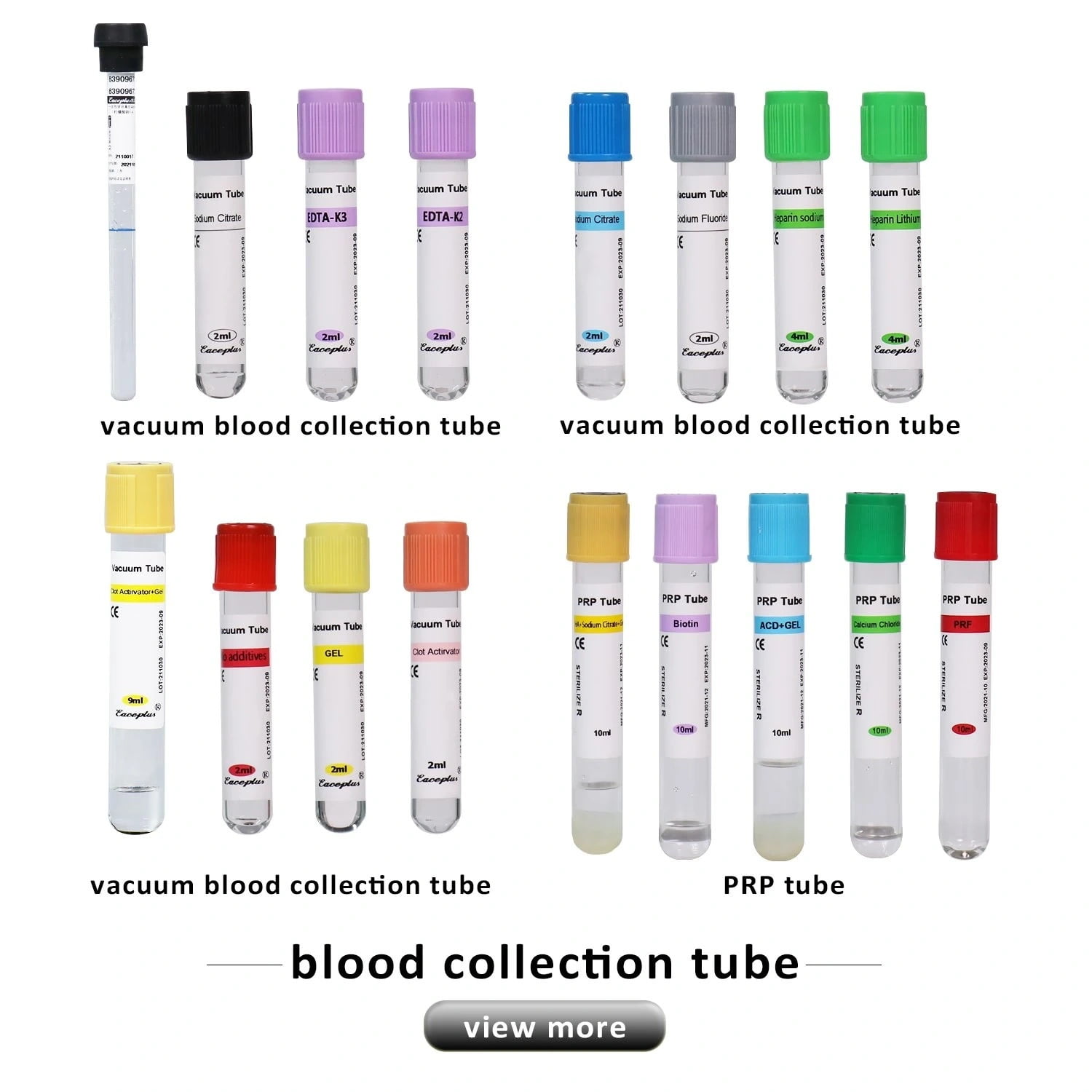
Blood collection is a crucial step in medical diagnostics, ensuring accurate test results and proper sample preservation. Blood collection tubes come with different additives, including anticoagulants, which prevent blood clotting and help in various laboratory analyses.
Choosing the right anticoagulant depends on the test type, as some require whole blood, plasma, or serum. In this detailed guide, we’ll explore the different anticoagulants used in blood collection tubes, their functions, and their specific applications in clinical and laboratory settings.
For high-quality blood collection tubes, visit Siny Medical, a trusted provider of laboratory and medical consumables.
Table of Contents
- 1 Why Are Anticoagulants Used in Blood Collection Tubes?
- 2 Types of Anticoagulants in Blood Collection Tubes
- 3 Anticoagulants in Blood Collection Tubes
- 4 When Choosing a Blood Collection Tube
- 5 Final Thoughts
- 6 FAQs
- 6.1 What is the purpose of anticoagulants in blood collection tubes?
- 6.2 How do different anticoagulants affect blood test results?
- 6.3 Why is EDTA the preferred anticoagulant for hematology tests?
- 6.4 How does heparin work as an anticoagulant?
- 6.5 Why is sodium citrate used for coagulation studies?
- 6.6 What is the function of fluoride in gray-top tubes?
- 6.7 Can anticoagulants alter blood chemistry results?
- 6.8 What is the difference between serum and plasma in blood testing?
Why Are Anticoagulants Used in Blood Collection Tubes?
Blood naturally clots when exposed to air, which can interfere with laboratory tests that require whole blood or plasma. Anticoagulants are added to blood collection tubes to prevent clotting and preserve the sample’s integrity.
Each anticoagulant serves a unique purpose, depending on the type of test being conducted:
- Some preserve blood cells for complete blood counts (CBCs).
- Others separate plasma for biochemical testing.
- Certain anticoagulants help in coagulation studies.
The selection of the anticoagulant is critical to obtaining accurate results. Below, we’ll examine the most commonly used anticoagulants in blood collection tubes.
Types of Anticoagulants in Blood Collection Tubes
EDTA (Ethylenediaminetetraacetic Acid) – Purple/Lavender Top Tube
Function:
EDTA tube is a chelating agent that binds calcium, preventing blood from clotting. It is widely used for hematology tests.

Common Uses:
- Complete Blood Count (CBC)
- Blood Smear Examination
- Hematology Research
Advantages:
- Preserves cell morphology for accurate microscopic analysis.
- Prevents platelet clumping.
To purchase EDTA tubes, visit Siny Medical.
Heparin – Green Top Tube
Function:
Heparin tubes acts as an anticoagulant by enhancing antithrombin III, which inhibits clotting factors. It is commonly used in plasma biochemical tests.

Common Uses:
- Electrolyte Testing
- Arterial Blood Gas Analysis
- Immunophenotyping
Advantages:
- Does not affect ion balance in electrolyte testing.
- Allows rapid plasma separation.
To learn more about heparin tubes, check out Siny Medical.
Sodium Citrate – Blue Top Tube
Function:
Sodium citrate binds calcium in the blood, preventing clot formation. It is primarily used for coagulation studies.
Common Uses:
- Prothrombin Time (PT) & INR Tests
- Activated Partial Thromboplastin Time (aPTT)
- Coagulation Factor Analysis
Advantages:
- Provides precise coagulation measurements.
- Easily reversible with calcium addition.
For sodium citrate tubes, visit Siny Medical.
Fluoride Oxalate – Gray Top Tube
Function:
Fluoride inhibits glycolysis, while potassium oxalate acts as an anticoagulant by binding calcium.
Common Uses:
- Glucose Testing
- Lactate Measurement
Advantages:
- Prevents glucose metabolism, ensuring accurate sugar level readings.
- Ideal for diabetes testing.
Find fluoride oxalate tubes at Siny Medical.
Anticoagulants in Blood Collection Tubes
| Anticoagulant | Tube Color | Primary Use | Mechanism of Action |
|---|---|---|---|
| EDTA | Purple/Lavender | Hematology (CBC) | Chelates calcium |
| Heparin | Green | Biochemistry | Inhibits clotting factors |
| Sodium Citrate | Blue | Coagulation Tests | Binds calcium |
| Fluoride Oxalate | Gray | Glucose Testing | Inhibits glycolysis |
When Choosing a Blood Collection Tube
When selecting a blood collection tube, consider the following:
- Type of test required – Different anticoagulants serve different diagnostic purposes.
- Sample stability – Some additives preserve blood better for long-term analysis.
- Interference with test results – Certain anticoagulants can alter chemical balances in tests.
For expert recommendations on blood collection tubes, contact Siny Medical.
Final Thoughts
Anticoagulants in blood collection tubes play a vital role in medical testing by preventing blood clotting and ensuring sample accuracy. Each type serves a unique function, from hematology to biochemical analysis.
For premium-quality blood collection tubes, explore Siny Medical. You can also check out their YouTube channel or visit their Made-in-China page for more information.
Looking for the best medical consumables? Contact Siny Medical today!
FAQs
What is the purpose of anticoagulants in blood collection tubes?
Anticoagulants prevent blood from clotting inside the collection tube, ensuring that samples remain suitable for laboratory testing. They are essential for tests that require plasma or whole blood, as clotting can interfere with accurate test results and lead to sample rejection.
How do different anticoagulants affect blood test results?
Each anticoagulant interacts with blood differently. For example, EDTA preserves blood cells for hematology tests, while heparin is ideal for plasma chemistry tests. Using the wrong anticoagulant can lead to inaccurate results, altered chemical balances, or sample clotting, affecting the reliability of laboratory analyses.
Why is EDTA the preferred anticoagulant for hematology tests?
EDTA prevents clotting by binding calcium, preserving blood cell morphology for microscopic examination. It ensures accurate Complete Blood Count (CBC) results by preventing platelet aggregation and maintaining red and white blood cell integrity, making it the standard choice for hematology tests worldwide.
How does heparin work as an anticoagulant?
Heparin enhances antithrombin III activity, inhibiting clotting factors like thrombin and factor Xa. This prevents blood from clotting inside the tube, making it ideal for plasma-based biochemical tests. Unlike EDTA, heparin does not significantly alter cell morphology, which is why it is used for specific diagnostic tests.
Why is sodium citrate used for coagulation studies?
Sodium citrate prevents clotting by binding calcium, an essential factor in the coagulation process. This makes it ideal for tests like Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT). Since its effect is reversible with calcium addition, it ensures precise coagulation measurements.
What is the function of fluoride in gray-top tubes?
Fluoride prevents glycolysis, ensuring accurate glucose measurements by stopping blood cells from metabolizing sugar. Potassium oxalate, the anticoagulant in gray-top tubes, binds calcium to prevent clotting. Healthcare professionals commonly use this tube for diabetes testing and lactate measurements.
Can anticoagulants alter blood chemistry results?
Yes, certain anticoagulants can interfere with blood chemistry. For example, EDTA increases potassium levels and decreases calcium, which may lead to inaccurate electrolyte readings. Heparin is preferred for biochemical tests because it does not significantly alter electrolyte concentrations. Choosing the correct tube is crucial for valid results.
What is the difference between serum and plasma in blood testing?
Serum is the liquid portion of blood after clotting, while plasma is the liquid portion that contains clotting factors, achieved by using anticoagulants. The laboratory utilizes plasma for tests that involve clotting factors, whereas serum is the preferred choice for biochemical tests, including liver and kidney function assessments.